My program of research examines psychosocial influences on health, particularly cardiovascular diseases, with an emphasis on Hispanic/Latino health and health disparities. Within this broad program I am currently devoting significant effort to 2 specific lines of inquiry: 1) examining social vigilance as a basic biobehavioral mechanism in stress and cardiovascular disease risk, and 2) understanding Hispanic/Latino health disparities, particularly the Hispanic/Latino mortality paradox.
Stress and Cardiovascular Disease
Social Vigilance is one candidate behavior potentially linking stress and a broad array of individual, social, and contextual stress moderators to CHD (see Figure 1). Social vigilance refers to the act of monitoring the social environment for potential interpersonal challenges or threats as well as monitoring change in status of a perceived threat.
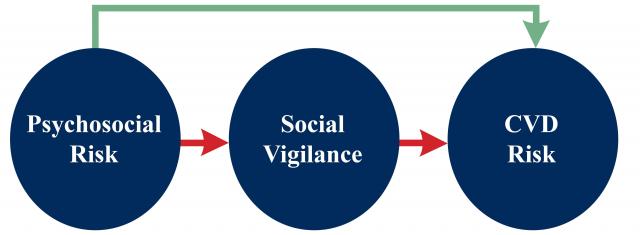
Figure 1: Social vigilance as a biobehavioral mediator of psychosocial factors on CVD risk.
People may engage in vigilant behavior for a variety of reasons including environmental factors (e.g., dangerous/threatening neighborhoods), social roles (e.g., jobs in security, caregivers), and individual differences (e.g., negative personality traits, stigma). Although adaptive in some circumstances, sustained vigilance or hypervigilance suggests a state of chronic stress which may have important health consequences. My collaborators and I have demonstrated that:
- Vigilance is a common behavior
- Vigilant behaviors varies as a function of the individual and the social environment
- Vigilance is associated with health-relevant personality traits (e.g., hostility, negative affectivity)
- Social vigilance is linked to known cardiovascular risk factors and hypothesized disease mechanisms
Ongoing Projects
- Determining social moderators of vigilance and cardiovascular/ autonomic reactivity
- Examination of discrimination as a moderator of vigilance and acute cardiovascular responses
- Measure development and validation
- Examining associations between vigilance and atherosclerotic risk The North Texas Heart Study
Hispanic Mortality Paradox
Emerging data across illness domains suggest that Hispanics experience better health than non-Hispanics, despite a significantly worse risk factor profile; this phenomenon is commonly referred to as the Hispanic Paradox. Perhaps the most striking aspect of this advantage is evidence that Hispanics live longer than NH Whites. We recently published a systematic review and meta-analysis of the longitudinal literature to address the longstanding debate over the validity of this phenomenon. The investigation encompassed 58 studies (4,615,747 participants) and found a 17.5% lower risk of mortality among Hispanics relative to other racial/ethnic groups. (Ruiz, Steffen, & Smith, 2013).
Conceptually, the observed mortality advantage may be due to better outcomes at various points in the illness course (see figure 2), including survival and recovery from acute events. For example, we recently demonstrated that Hispanics experience better in-hospital survival and lower lengths of stay compared to non-Hispanics after controlling for age, gender, and reason for admission (Ruiz, Hamann, et al., 2014). Much of my current work is now focused on further deconstructing the paradox with the goal of identifying cultural forms of resilience.
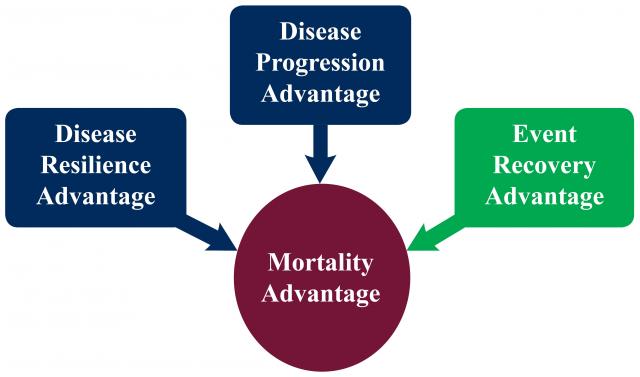
Figure 2: Conceptual deconstruction of the Hispanic/Latino mortality advantage.
![]() University of North Texas, 1155 Union Circle # 311280, Denton, TX 76203
University of North Texas, 1155 Union Circle # 311280, Denton, TX 76203 ![]() 1611 W. Mulberry/ Terrill Hall, Room No.: 351
1611 W. Mulberry/ Terrill Hall, Room No.: 351![]() john.ruiz@unt.edu
john.ruiz@unt.edu ![]() 940.369.8228
940.369.8228